Abstract
Introduction: Infections are a significant cause of hospitalizations, morbidity, and mortality in multiple myeloma (MM) patients. The aim of this study was to determine the efficacy of intravenous immunoglobulin (IVIG) prophylaxis in reducing infection-related hospitalizations (IHs) in MM patients.
Methods: This was a retrospective study of MM patients who received IVIG at Taussig Cancer Center between July 2009 and July 2021. IVIG was initiated at the discretion of the treating oncologist based upon serologic hypogammaglobulinemia (HGG) and recurrent infections. Patients received IVIG at doses of at least 0.4mg/kg every 30 to 60 days during periods of IVIG. The duration of each period of IVIG was determined by the treating oncologist based upon recovery of serum IgG levels. Patients could require multiple periods of IVIG and there could be intervals of months to years between periods of IVIG. Data was collected from 1 year prior to a patient's first IVIG period to 1 year after their last IVIG period. A patient's study period was divided into time "on-IVIG" and time "off-IVIG": the 60-days following a dose of IVIG was categorized as on-IVIG while all other time periods were categorized as off-IVIG. IHs were labeled as occurring on-IVIG or off-IVIG if the infection was initially diagnosed while the patient was on-IVIG or off-IVIG. Patients who did not have at least 60 days on-IVIG, 30 days off-IVIG and 1 IH during their study period were excluded.
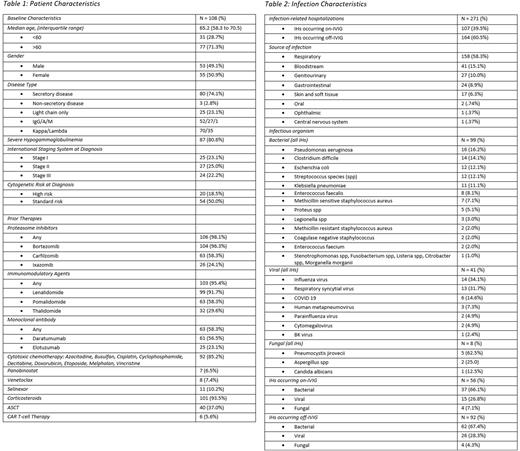
Data was collected on baseline patient characteristics, MM disease characteristics, treatment history, IVIG administration and infection characteristics. Severe HGG (sHGG) was defined as serum IgG levels <400 mg/dL. Patients were labeled as having a 1 year period of continuous IVIG if they received a dose of IVIG at least every 60 days for 365 days. Cytogenetic risk was defined using the International Myeloma Working Group criteria. The primary endpoint was the rate of IHs per patient-year on-IVIG vs. off-IVIG. Secondary endpoints were mean length of hospital stay and ICU stay for IHs on-IVIG vs. off-IVIG. Continuous and categorical variables were analyzed using paired t-test and chi-squared test respectively.
Results: Of 395 patients who were screened, 108 were included. Novel agent exposure was broad and included proteasome inhibitors (106, 98.1%), immunomodulatory drugs (103, 95.4%) and monoclonal antibodies (63, 58.3%). Patients spent a total of 81,871 days on-IVIG and 71,303 days off-IVIG with each patient spending a median 758 days on-IVIG and 660 days off-IVIG. There were 271 total IHs in the study with 107 (39.5%) occurring on-IVIG and 164 (60.5%) occurring off-IVIG. Of the 271 total IHs, respiratory was the most common infectious source (158, 58.3%). 20 (18.7%) of the 107 IHs that occurred on-IVIG required intensive care unit (ICU) stay while 30 (18.3%) of the 164 IHs that occurred off-IVIG required ICU stay.
There was a significant difference in the primary endpoint of rate of IHs per patient-year on-IVIG vs. off-IVIG in the overall study population (.81 vs. 1.08; Mean Difference [MD], -.27; 95% Confidence Interval [CI], -.57 to .03; P value [P] = .04). Subgroup analysis showed that patients with a 1 year period of continuous IVIG (49, 45.3%) had a significant reduction in IHs per patient-year while on-IVIG vs. off-IVIG (.48 vs. .78; MD, -.30; 95% CI, -.59 to .002; P = .03). The subgroup with standard-risk cytogenetics (54, 50.0%) and the subgroup with 2 or more IHs (67, 62.0%) also showed a significant reduction in IHs while on-IVIG vs. off-IVIG (.65 vs. 1.01; MD, -.36; 95% CI, -.71 to -.01; P = .02) and (1.04 vs 1.43; MD, -.39; 95% CI, -.82 to .05; P = .04) respectively. The subgroup with sHGG (87, 80.6%) and the subgroup with high-risk cytogenetics (20, 18.5%) did not show a significant reduction in IHs while on-IVIG vs. off-IVIG (.79 vs. 1.05; MD, -.26; 95% CI, -.60 to .07; P = .06) and (1.17 vs. 1.01; MD, .16; 95% CI, -.75 to 1.07; P = .64) respectively. For the secondary endpoints of mean length of hospital stay and ICU stay, there was no significant difference between IHs occurring on-IVIG vs. off-IVIG (6.4 days vs. 6.3 days; MD, .10; 95% CI, -1.2 to 1.4; P = .55) and (4.3 days vs. 5.2 days; MD -.90, 95% CI, -3.0 to 1.1; P = .18) respectively.
Conclusion: IVIG showed significant benefit in reducing infection-related hospitalizations in the overall population and in multiple subgroups. IVIG should be considered in certain cohorts of MM patients to prevent infection-related hospitalizations.
Disclosures
Anwer:Janssen: Consultancy; Allogene Therapeutics: Research Funding; BMS: Consultancy, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal